
Mr. Sebastianelli with Dr. Vale after a recent follow-up. He has made a full recovery following treatment with amniotic membrane

Mr. Lombardi with Dr. Vale during a recent exam. Amniotic membrane transplant fixed a PED that was present for almost 10 months.
Dr. Vale recently performed amniotic membrane transplantation on two gentleman suffering persistent epithelial defects (PEDs) of the cornea, saving their eyes and their vision. This revolutionary treatment option is offered at both the Lehigh Valley and Scranton offices of InterMountain Eye Associates by Dr. Steven Vale and his staff. Call today if you are suffering from this sight threatening condition or if you have had recurrent episodes of persistent epithelial defects of the cornea that have been resistant to treatment. Relief is in sight for your corneal problem at InterMountian Eye Associates!
About PEDs
Persistent corneal epithelial defect (PED) is a spectrum of degenerative diseases of the cornea caused by an impairment or loss of function of the ophthalmic branch of the trigeminal nerve, the sensory nerve of the eye. Loss or impairment of corneal sensory innervation is the most common cause of persistent, non-healing corneal epithelial defects, which can lead to corneal scars that degrade vision, or worse, ulceration and even perforation of the cornea (a hole in the eye!).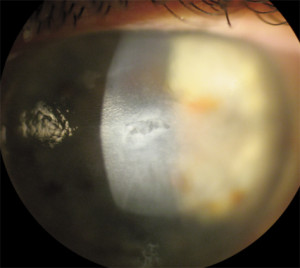
Diagnosis
- History: May include previous herpes simplex virus (HSV) keratitis, herpes zoster ophthalmicus (HZO), diabetes, brain or facial surgery, trauma to the head or face, or prior radiation exposure.
- Symptoms: Patients often have blurry vision, may have a red eye, but often with minimal discomfort unless the eye has already perforated.
- Examination: Central or paracentral corneal epithelial defect (with dye staining), often with thinning or dissolving tissue (corneal melt), infrequent blinking, decreased corneal sensation, and low tear lake.
- Microbiological examination may need to be performed to exclude bacterial, fungal, or viral infections when there is an inflammatory infiltrate present.
Treatment Strategy
- Restore corneal integrity by reducing inflammation, promoting healing, and preventing haze together with tarsorrhaphy to keep the surgical site covered
- Treat underlying cause (e.g., antivirals, antibiotics)
- Treat associated dry eye (punctal occlusion, tears, ointments)
- Prevent further damage (withdraw unnecessary topical drugs)
- Reduce the risk of secondary infections (keeping the eyelids clean, antibiotics)
When the cornea loses the ability to sense pain, dryness or injury, there is significant danger of loss of vision or even blindness. This condition is known as neurotrophic PED. Neurotrophic PED is also characterized by decreased corneal sensation, epithelial breakdown, and poor healing. Co-existing eye surface diseases such as dry eye, exposure keratitis, and limbal stem cell deficiency may be present and worsen the prognosis. The disease progression is often asymptomatic and can lead to corneal infection and melting/perforation if not treated promptly. Conventional treatments such as preservative free tears, medicated ointments, bandage contact lenses, tarsorrhaphy and even autologous blood serum eyedrops often fail at promoting prompt healing and tend to result in corneal scarring if healing is delayed.
Amniotic membrane is tissue that is taken from the placenta newborn babies. It undergoes extensive sterilization and preparation to assure it is virus and bacteria free before it is cryopreserved or lyophilized and then modified into discs or tissue squares which can be placed or surgical adhered to the ocular surface. Amniotic membrane contains epithelial and nerve growth factors (NGF), which facilitates epithelial healing and helps recover corneal sensitivity.
Surgical transplantation of amniotic membrane by Dr. Vale saved these gentlemens’ vision. Let Dr. Vale help you too. Call today for a comprehensive evaluation by the doctor.
Comments are closed