Meibomian Gland Dysfunction (MGD) and Meibomianitis are Common Causes of Dry Eyes…
These Conditions often respond well to a multi-step therapeutic regimen. In various combinations, lid hygiene, warm compresses, lid margin compression, Omega-3 fatty acids and medication can all offer benefits.

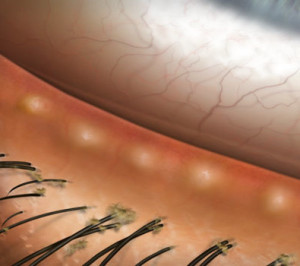
On the superior eyelid, dilated and inspissated meibomian glands are visible. Note the multiple glands that are affected (above). Red, thickened lid margins are also noticable
Patients often present to InterMountain Eye Associates for routine eye care with nonspecific complaints of ocular discomfort. By examining the lid margins, we often can identify the cause of a patient’s comfort issues. Meibomian gland dysfunction (MGD) can lead to inflammation of the meibomian glands (meibomianitis) and poor quality or deficient oil in the tear film. Bacteria and their fat dissolving enzymes often accompany the oil, which causes a myriad of ocular surface complaints and signs. Here is a review of the common causes of and treatments for meibomian gland dysfunction to help you understand this common condition.
The Meibomian Glands
Meibomian glands are modified sebaceous glands that are arranged vertically within the tarsal plate (inside the eyelid). There about 30 such glands on the upper lid margin and about 25 on the lower lid margin of each eye. These glands secrete and oil known as Meibum. The interactive force of an eyelid blink and the contraction of a linear muscle that runs through the lid margin, the Muscle of Riolan, causes meibum to be excreted onto the posterior lid margin. This oil initially protects the eyelids from maceration and creates a seal when the eyes are closed. As meibum interacts with the tear film, it reduces surface tension and enhances the tears by spreading them evenly, supporting a clear refractive interface and maintaining a consistent quality of vision. The oil also covers the tear film, thereby slowing the rate of tear evaporation. A good analogy would be the puddle in the parking lot of Wal-Mart that doesn’t evaporate even on the hottest day of the year, because it is covered with motor oil from the cars that leak oil onto the lot.
Meibomian Gland Dysfunction (MGD)
Meibomian gland dysfunction may occur because of changes in oil production as we age, as a result of poor diet, as a consequence of skin disorders such as rosacea or seborrheic dermatitis, or even because of poor facial and eyelid hygiene. With Meibomian gland dysfunction, patients may initially be asymptomatic, but eventually vision is affected because there is poor quality oil or too little oil in the tear film. This disturbance causes tear film instability, high tear osmolality (too salty tears) and rapid tear evaporation. Though dry eye itself may be caused by the excessive tear evaporation, the inflammation involved with dry eye irritation is actually worsened by the tears being too salty, i.e. the inflammatory process is initiated by the high salt content of the tear film.
Meibomianitis
Meibomianitis or Meibomitis, also termed posterior blepharitis, is the most common form of lid margin disease (LMD); nearly 40% of routine eye care patients and 50% of contact lens wearers are affected. Meibomianitis may cause or exacerbate dry eye-like symptoms. Dryness, itching, stickiness, foreign body sensation, burning, watering, photophobia and intermittent blurred vision are frequently seen in cases of meibomitis.
Meibomianitis can exist alone, or it can be associated with anterior blepharitis or seborrheic dermatitis

Here, inspissation of the meibomian gland secretions is so great that the glands are actually plugged by thickened, hard meibum and the lid margins show marked telangectasias
• Primary meibomianitis. Also known as obstructive MGD, primary meibomianitis is a generalized dysfunction of the sebaceous glands. It is commonly associated with acne rosacea, acne vulgaris and seborrheic dermatitis. The anterior lid margin typically appears abnormal in those with primary meibomianitis, with the meibomian glands dilated and blocked with inspissated secretions that are sluggish or stagnant upon expression. There is often an associated dilation of the eyelid blood vessels, known as telangiectasias. These changes cause a red, beefy appearance to the eyelids margins. The conjunctiva, the normally clear lining over the white of the eye may be injected, giving a red or pink eye appearance.
• Anterior blepharitis. This bacterial infection of the lash line can lead to secondary infection and inflammation of the adjacent meibomian glands. In addition to the typical signs of anterior blepharitis, dry scales at the base of the lashes, known as collarettes, focal patches of inflamed or plugged meibomian glands may be evident. It is unclear if bacteria cause the glands’ secretions to become thickened (i.e., inspissated), or if they simply exacerbate the condition by causing inflammation. But, it is known that gram-positive bacteria, such as S. epidermidis and S. aureus, release lipases that break down sebaceous gland lipids. These enzymes produce free fatty acids and other by-products that irritate the eyes and cause tear film instability.

Seborrheic blepharitis with the classic scurf on the lashes
• Seborrheic blepharitis. Patients with seborrheic dermatitis (a skin condition that affects the sebaceous glands of the scalp, face and eyebrows) often also have scurf, which are greasy flakes on the lashes, and have inflamed or infected lid margins. The condition is then known as seborrheic blepharitis. These patients may simply have increased meibomian secretions, or meibomian seborrhea. Along with the greasy scales seen in the lashes, excess meibomian oil is usually evident on the lid margins and in the pre-corneal tear film. The meibomian glands are dilated and full of meibum that can be easily expressed. Frequently, soapy-looking bubbles are seen along the inferior lid margin. This saponification occurs when excess lipid secretions react with protein in the tears. Patients with meibomian seborrhea frequently complain of burning upon awakening. The condition is similar to getting soap in one’s eyes. Inflammation is usually minimal in cases of meibomian seborrhea, so patient symptoms are often worse than observed signs. The localized inflammatory response that results from meibomian stasis can lead to permanent keratinization and scarification of the meibomian glands. Such an advanced condition affects the lid margin contour and gland placement, as the opening to the glands migrate posteriorly as the lid margin becomes effaced. Due to a lack of oil in the tear film, these patients typically have a reduced tear film breakup time (TBUT) and increased tear evaporation rates.
Early Signs of MGD
It is easy to dismiss the subtle signs of early MGD. Looking for oily lid margins, excess oil in the tear film, dilated meibomian glands, mild injection and the occasional inspissated gland helps to make the diagnosis. Even if patients are asymptomatic, it’s not too early to start educating them about lid hygiene, the chronicity of the condition, and possible sequelae if left untreated. In cases of longstanding disease, signs include thickened (tylotic) eyelid margins, telangiectatic vessels, loss of lashes (madarosis), poliosis, trichiasis and notching of the lid margin. Chronically inspissated glands eventually become keratinized and “drop out,” leaving a divot in the lid margin. This causes a shift in position of the remaining meibomian glands, and they become unable to secrete oil onto the proper location of the lid, which results in permanent changes in the tear film composition and ocular environment, and significant dry eye symptoms.
Care for MGD Patients
A happy patient who sees well is the goal of the eye care professionals at InterMountain Eye Associates. In MGD patients, the reduction of symptoms is important, and the prevention of permanent damage that can affect the eye’s ability to maintain a balanced environment is paramount. Many effective treatments for MGD are available, so therapeutic care may be tailored to each patient. Patients should recognize the signs and symptoms of meibomian gland dysfunction and understand that MGD is a chronic condition that requires a regular, if not daily, lid hygiene regimen. Treatment should incorporate lid hygiene techniques with expression, if possible. As with any chronic disease, continued compliance is a challenge for patients and doctors alike. Luckily, most of the following treatments are not difficult to perform or explain:
• Lid scrubs. These help to remove oil, bacteria and debris, as well as to stimulate the meibomian glands. Baby shampoo or mild soap have historically been recommended to patients with seborrheic f orms of lid disease. Note that some patient’s eyes are sensitive and become chemotic and injected due to the detergent. OcuSoft (OcuSoft) and SteriLid (Advanced Vision Research) are bactericidal products available commercially. These products may be less irritating to the conjunctiva than shampoo or soap. Lid scrubs may be prescribed at different steps within the lid hygiene regimen. In patients with anterior blepharitis, lid scrubs should be performed before massage so the lashes are cleared of bacteria and debris prior. In patients with posterior blepharitis, one may opt to first express meibum from deep within the lids, then perform lid scrubs to remove excess oil.
orms of lid disease. Note that some patient’s eyes are sensitive and become chemotic and injected due to the detergent. OcuSoft (OcuSoft) and SteriLid (Advanced Vision Research) are bactericidal products available commercially. These products may be less irritating to the conjunctiva than shampoo or soap. Lid scrubs may be prescribed at different steps within the lid hygiene regimen. In patients with anterior blepharitis, lid scrubs should be performed before massage so the lashes are cleared of bacteria and debris prior. In patients with posterior blepharitis, one may opt to first express meibum from deep within the lids, then perform lid scrubs to remove excess oil.
• Warm compresses. Heating the lids about 110ºF significantly increased meibomian oil production and liquidity. Using warm compresses, heat should be applied to the eyes for 4 to 10 minutes. This warms the meibum, allowing it to flow more freely, and helps soften lash debris. Many eye doctors recommend patients perform compress therapy with a wet washcloth towards the end of a hot shower. This should encourage compliance by helping incorporate lid hygiene into the daily routine and may also enhance the therapeutic effect since meibomian glands and skin pores open in a hot shower. Other warm compress methods are a microwaved sock filled with dry rice, hot hard-boiled eggs in a damp sock, and microwave heated gel-filled masks under a hot washcloth. After the application of warm compresses, patients with all forms of posterior blepharitis should massage their lids to help express meibum from deep within the glands.
• Lid Margin Compression. Lid compression and massage can dramatically improve symptoms by helping re-establish tear film stability. Research has demonstrated that, after gland expression, TBUTs return to normal, and in some cases, super-normal levels.
The technique: Extend a clean finger and apply light pressure directly to the lid margin, as close to the lid margin as possible. Apply upward pressure on the lower lid margin while in upgaze, walking the fingertip along the entire lid margin and overlapping the area just compressed. Repeat with the upper lid, applying downward pressure to the margin as you walk the fingertip along the upper lid margin. Repeat for the other eye.
Excessive manipulation of the lids can cause additional irritation, so lid massage and scrubs should be performed twice a day during the acute stage, and may be decreased to once daily during maintenance. Follow-up care is important in these cases, so that treatments can be assessed and modified. After regular lid hygiene, have patients instill an artificial tear. This helps to rinse away the extra oil from gland expression and/or any residue from the lid scrub. MGD patients also typically have dry eye, so tears are often recommended between two and four times per day.
Medications for MGD Patients
Medications are reserved for acute or recalcitrant cases. Because of the common comorbidity of MGD and dry eye, patients are often on dry eye therapy while on MGD treatment. Restasis (cyclosporine 0.05%, Allergan) may be especially beneficial for those who suffer from aqueous deficient or inflammatory dry eye. A recent study found that dry eye patients on Restasis had fewer meibomian gland inclusions and less lid margin injection. Restasis is especially effective in those with acne rosacea and meibomian gland dysfunction.
 Omega-3 fatty acids. Found in fish oils and flaxseed are commonly recommended to patients with dry eye, meibomian gland dysfunction or meibomianitis. They are polyunsaturated fats and result in the meibomian glands producing a less viscous meibum the flows better. Omega-3 fatty acids also have anti-inflammatory effects. For a link that details the benefits of fish oil, Click Here.
Omega-3 fatty acids. Found in fish oils and flaxseed are commonly recommended to patients with dry eye, meibomian gland dysfunction or meibomianitis. They are polyunsaturated fats and result in the meibomian glands producing a less viscous meibum the flows better. Omega-3 fatty acids also have anti-inflammatory effects. For a link that details the benefits of fish oil, Click Here.
 Tetracyclines. For ongoing management of MGD, tetracyclines are effective and useful. Oral tetracyclines—e.g., doxycycline and minocycline—appear to inhibit bacterial lipase production. This reduces free fatty acids, which helps to lessen inflammation and symptoms of irritation. Tetracyclines also help inhibit keratinization of the meibomian glands, and have been shown to reduce the number of Staphylococcus organisms. Ocular hygiene kits that package tetracyclines and hygiene tools together for patients are now available for prescription. Side effects can be kept at a minimum with a decreased dose of tetracyclines. Minocycline is often used by our practice, because it already carries a lower dosage option (50mg), once-a-day treatment, and few side effects (particularly with regards to sun exposure). Patients may be kept on a maintenance dose as long as necessary.
Tetracyclines. For ongoing management of MGD, tetracyclines are effective and useful. Oral tetracyclines—e.g., doxycycline and minocycline—appear to inhibit bacterial lipase production. This reduces free fatty acids, which helps to lessen inflammation and symptoms of irritation. Tetracyclines also help inhibit keratinization of the meibomian glands, and have been shown to reduce the number of Staphylococcus organisms. Ocular hygiene kits that package tetracyclines and hygiene tools together for patients are now available for prescription. Side effects can be kept at a minimum with a decreased dose of tetracyclines. Minocycline is often used by our practice, because it already carries a lower dosage option (50mg), once-a-day treatment, and few side effects (particularly with regards to sun exposure). Patients may be kept on a maintenance dose as long as necessary.
Comments are closed